Chronic pain is a condition requiring comprehensive management Patients with this condition may have already been through the traditional medical system with blood tests, x-rays, MRI’s, and injections, and yet they still don’t have an answer to what is going on with their body. A diagnosis or multiple diagnoses may be made – fibromyalgia, disc herniation, lumbago, cervicalgia, stenosis, arthritis – but treatment of the diagnosed conditions doesn’t change the pain. Perhaps because treatment is missing the point. If your pain system itself is messed up, no treatment will fix the pain until the pain system is treated.
How Do Nerves Work With Chronic Pain (or How Is the Nervous System Like a Business)?
Let’s picture the nervous system like a company. The brain is the CEO of the company, the department managers are the spinal cord, and all of the nerves in the body are the workers. In a normal company, messages get sent from the workers to the managers, and if the message is important enough it will get sent to the CEO. When the CEO gets the message it fixes the problem and things go back to normal.
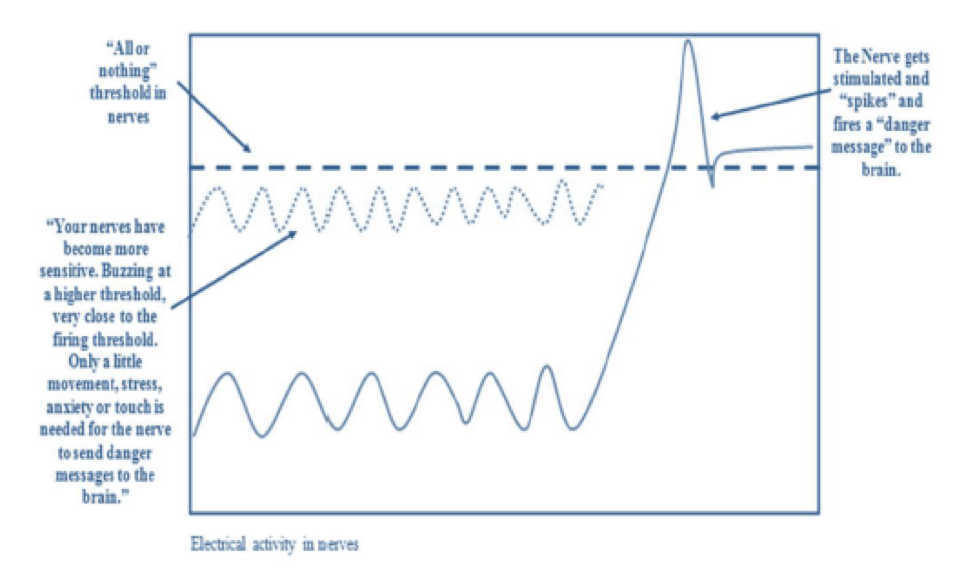
However, if a problem persists, the CEO starts to request more information, and instead of going through managers, they want the messages directly. Nerves work the same way in chronic pain patients. If a problem persists , the brain wants to know everything about the area, causing an increase in information to be relayed, what we call “sensitization” for the area. Below is a diagram describing how nerves can become overly sensitized.
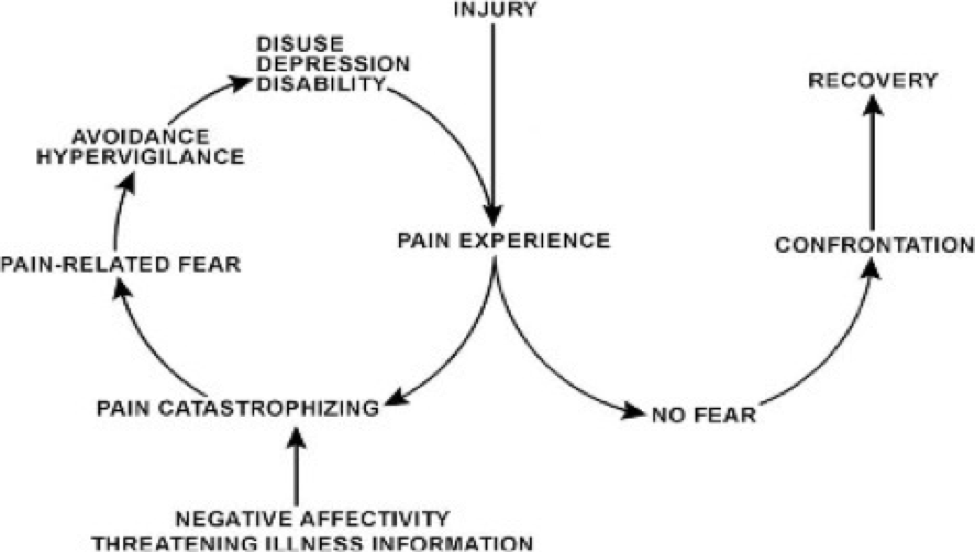
In the diagram you can see how the body’s wiring becomes dysfunctional. Your body and brain work together to become essentially an overprotective “guardian angel.” This guardian angel learned to “turn up the volume” of your pain and to over-guard your movement patterns to “protect” you from hurting yourself further. These adaptations are worsened or accelerated by stress – and who wouldn’t be stressed if they had pain all the time? So it’s a vicious cycle. This cycle is illustrated below.
Many factors affect the pain experience, including a busy environment, an increase in stress, failed past treatments, an increase in fear and anxiety, or social issues with family or work.
Treating the Pain System
Two treatment plans need to take place for you to heal; one of them addresses your headache or herniated disc or plantar fasciitis (or fill-in-the-blank.) The other one addresses fixing your pain system. Both of these areas must be treated for you to get better. The simple steps involve learning to calm your sympathetic (“fight or flight”) nervous system, modifying your behavior to reduce stress on your tissues while still staying active, normalizing impaired movement patterns (many of which you didn’t even realize you’ve developed) and following medical plans that support healing your pain system. Below is a list of ways that we treat your pain system.
Maximize The Power of Knowledge
- Just knowing that extra sensitive nerves create pain, and not necessarily an ongoing injury, can reduce nerve sensitivity. Knowledge of how the pain system works has been shown to decrease sensitization.
-
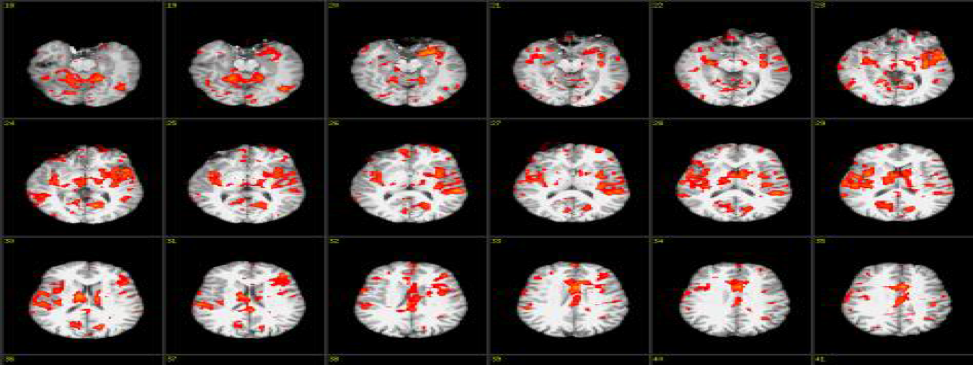
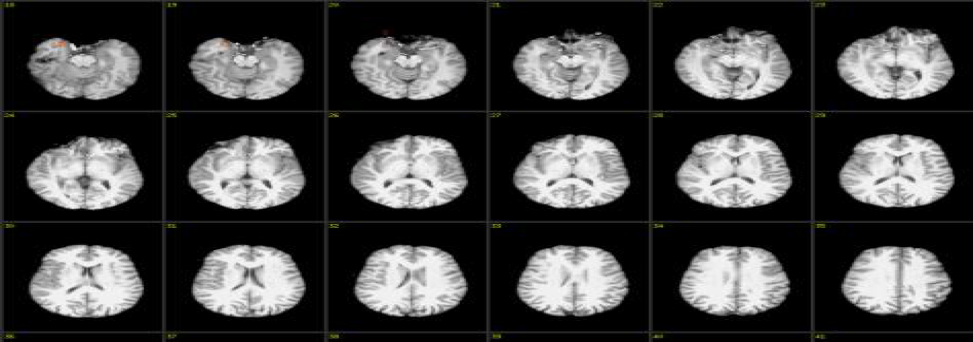 The fMRI pictures shown above demonstrate the brain activity before and after a 2.5-hour session about how the pain system works. As you can see the amount of brain activity affecting pain perception is markedly decreased from just knowing how things work.
The fMRI pictures shown above demonstrate the brain activity before and after a 2.5-hour session about how the pain system works. As you can see the amount of brain activity affecting pain perception is markedly decreased from just knowing how things work.Aerobic Exercise
Staying active while normalizing movement patterns is also important. Nerves love movement and exercise can get blood pumping, calming down nerve activity. Only 10-20 minutes a day is all that is needed to improve sleep, decrease stress, and decrease depression. If you are worried about starting to exercise, some strategies you can use involve starting small, taking breaks, making a plan, and setting goals.
Sleep Hygiene
Normalized sleep patterns get your body on a schedule and allow for recovery after a days work. It might be hard at first to find a normalized pattern, but some sleep strategies you can use include: making sure all of the lights are off, picking a consistent time to go to bed, avoiding naps and caffeine throughout the day, and doing some sort of exercise throughout the day.
The 5 Minute Summary!
This is a simple video put together by the National Health Performance Authority of Australia that is designed for Understanding Pain in Less than 5 minutes:
https://www.youtube.com/watch?v=C_3phB93rvI
What You Can Do
Many of our clients with persistent pain have already received some of this information from other practitioners along the way – but they haven’t been given the opportunity or resources to understand it. They feel labeled as “a chronic pain patient” or they feel as if no one is listening to them about their real pain; it is not “in their head!” So they look for more answers, a different diagnosis. Often “diagnosis” of the primary injury or condition is correct; it just hasn’t been treated in a comprehensive way. It hasn’t been treated with consideration of pain system repair or with a functional end in mind.
Resolving chronic pain is not easy, but as a wise professor told me, “hard is not bad; it’s just hard!” To get on the road to better health and a more normal life, seek out a support team, beginning with practitioners who are prepared to treat both your musculoskeletal problem and your pain system.
- References:
- Moseley G. Widespread brain activity during an abdominal task markedly reduced after pain physiology education: fMRI evaluation of a single patient with chronic low back pain. Aust J Physiother. 2005: 51(1):49-52. http://doi.org/10.1016/S0004-9514(05)70053-2.
- Moseley G, Nicholas M, Hodges P. A Randomized Controlled Trial of Intensive Neurophysiology Education in Chronic Low Back Pain. Clin Jour of Pain . 2004: 20(5): 324-330. http://dx.doi.org/10.1097/00002508-200409000-00007
- Coronado R, Bialosky J, Bishop M. The Comparative Effects of Spinal and peripheral Thrust Manipulation and Exercise on Pain Sensitivity and the Relation to the Clinical Outcome: A Mechanistic Trial Using a Shoulder Pain Mode. J Orthop Sports Phys Ther. 2015 Apr; 45(4);252-64. doi:10.2519/jospt.2015.5745.
- Louw A. Why do I hurt?. Minneapolis MN: Orthopedic Physical Therapy Products 2013