What’s Up with Shoulder Replacements?
First, you need to understand a little about the shoulder joint.
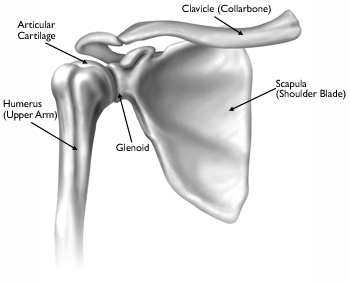
The humerus is the upper arm bone. It rests in the glenoid (the shoulder socket) which is part of the shoulder blade or the Scapula. This is referred to as the glenohumeral joint. Four muscles collectively known as the rotator cuff attach the scapula to the humeral head keeping the head of the humerus positioned correctly in the glenoid (the socket), providing stability while you move your arm. When someone has a rotator cuff tear, it is these muscles they are referring to.
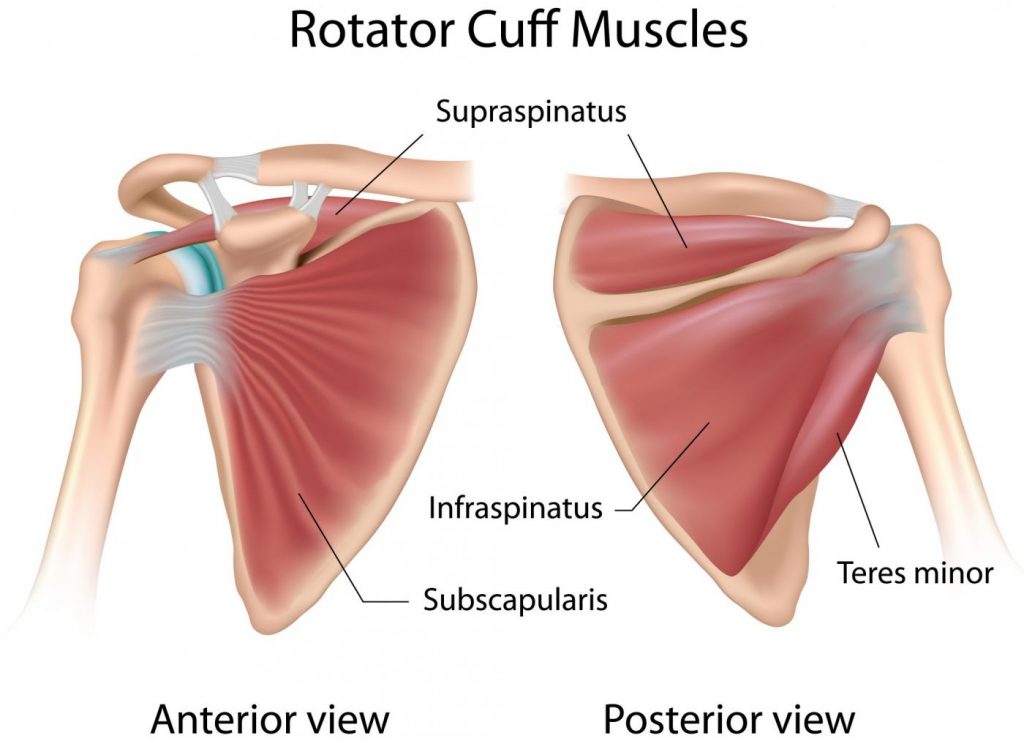 Those muscles can be seen in the picture and are listed in the order for the most commonly torn.
Those muscles can be seen in the picture and are listed in the order for the most commonly torn.
- Supraspinatus: Initiates the out to the side motion and stabilizes the humeral head against the glenoid.
- Infraspinatus: Stabilizes the shoulder and rotates the arm externally as if to throw a ball overhanded.
- Subscapularis: Rotates the shoulder inwardly while stabilizing the shoulder.
- Teres minor: Helps to externally rotate the shoulder and assist in reaching backward or reaching across your chest.
If you have pain in your shoulder and/or develop limited motion, how do you know what is going on? A trip to your doctor may result in an x-ray or an MRI. If the MRI shows a rotator cuff tear and or arthritis does that mean that is what is causing your pain? Maybe not. A study reported in the International Journal of Rheumatic Disease (2014: 17:863-871) conducted x-rays and MRIs on 30 older adults (over the age of 55), 10 with no history of shoulder pain, 10 with a history of shoulder pain and 10 with current shoulder pain. The radiographs showed evidence that all participants presented with similar shoulder abnormalities in similar proportions between all the groups. In a 2014 systematic review in the Journal of Shoulder and Elbow Surgery 30 studies were examined with a total of 6100 shoulders included and it found similar results. They concluded that clinical symptoms do not necessarily match radiological symptoms. Everybody gets degeneration of the rotator cuff muscle as they age. In other words, your shoulder looks bad on MRI or x-ray and you have pain, my shoulder shows the same deficits and feels fine. It is difficult to say if that arthritis or soft tissue damage is really the cause of the pain.
Physical therapy may be your best first step. PT can evaluate your motion and strength as well as the mechanics of how you move your arm. Then they will set up a program to address your deficits and provide you with exercises to do at home to supplement your time in PT. You may eliminate the need for surgery, but even if you get limited improvement having PT before your surgery may help in your rehab process afterward.
Now let’s look at the 3 types of shoulder replacement (referred to as shoulder arthroplasty).
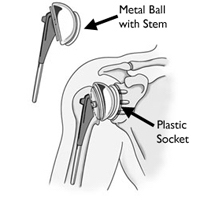
TOTAL SHOULDER REPLACEMENT (TSA): Replaces the humeral head, and the glenoid (the socket). It is set up in the same position as the original shoulder. This is great for those with severe arthritis in the whole shoulder and a mostly intact rotator cuff. It should provide relief from painful arthritis. The shoulder must still rely on the rotator cuff muscles to power the shoulder.
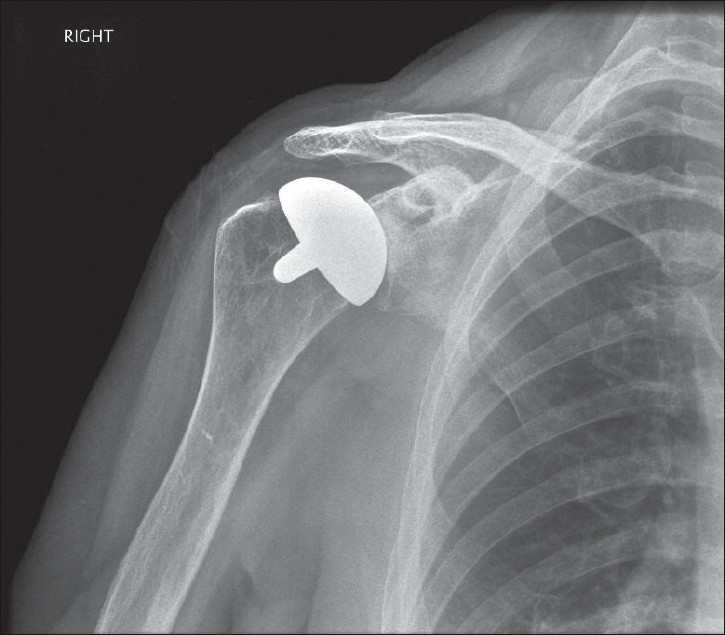
HEMI ARTHROPLASTY: Replaces only the humeral head. This may be done in cases where you severely fracture the humeral head, where arthritis is only on the humeral head but the glenoid has healthy and intact cartilage or where there is severe damage to the rotator cuff so a TSA is not appropriate.

REVERSE TOTAL SHOULDER (RTSA): Switches the alignment of the humeral head so the ball is attached to the scapula at the glenoid and the socket is placed at the head of the humerus. It is designed for those who have severe arthritis and loss of their rotator cuff muscle, those with no arthritis but severe weakness due to the torn rotator cuff, or someone who has had a failed total shoulder. For these folks, a normal TSA may not relieve their pain or allow them to lift their arm overhead or out to the side. The deltoid, the large triangular muscle at the top of the shoulder will take over the job of the rotator cuff muscles.
What happens after surgery?
Physical therapy will be crucial to your recovery after your shoulder replacement, no matter which surgery you have. The rehab for the hemiarthroplasty and the TSA will be the same, but rehab for the reverse shoulder is a little different. There is a higher risk for early dislocation in the reverse TSA so rehab must progress more slowly in the beginning. Patients can expect to have limited use of the shoulder in the first 4-6 weeks but should see rapid improvement in reduction of pain. Most patients are able to return to sports such as golf, tennis, swimming, and fitness sports within 6 months to a year. The TSA is anticipated to have the best results.
Listen to a podcast on Shoulder replacements click the link below:
http://www.moveforwardpt.com/radio/detail/total-shoulder-replacement-2
Or click on this link to read:
Physical Therapist’s Guide to Total Shoulder Replacement (Arthroplasty)
http://www.moveforwardpt.com/symptomsconditionsdetail.aspx?cid=4e1deb00-f6fd-40d4-b28c-28319f0d6d4a